The Post Heart Attack Stem Cell Treatment Consists of the Following:
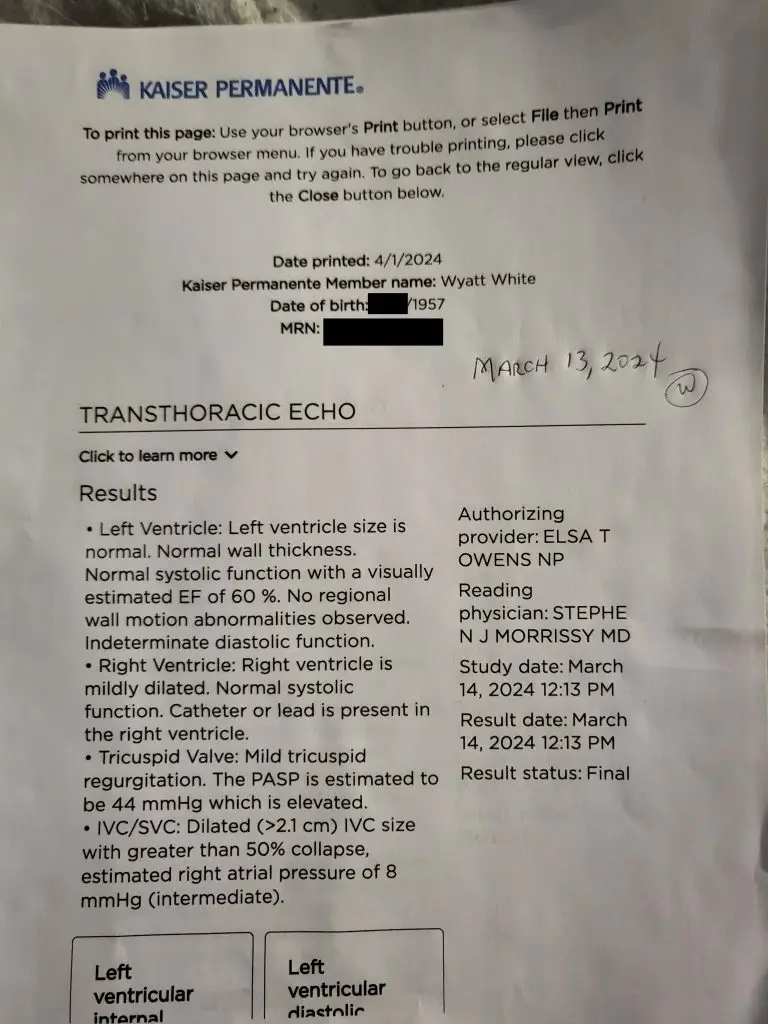
EKG, Echocardiogram, chest x-ray then analysis with cardiologist and internist
300 Million Stem Cell IV
NAD+ and High Dose Vitamin C IV drip after the stem cells
PRICE: $11,800 USD
We require patients to be in town for at least 5 days. Below is what a typical schedule looks like, but exact details are subject to change depending on availability and schedule:
- Day 1: Arrive and Rest
- Day 2: Bloodwork, EKF, Echocardiogram, chest x-ray & Payment
- Day 3: Review scans with our Internist to clear you for treatment. (They reserve the right to deny treatment if they believe your heart can’t handle treatment). Then payment.
- Day 4: Take cells out of cultivation
- Day 5: Treatment
- Day 6: Fly Home (We recommend staying one more day to rest, but you can leave on this day
If you are in town for more than 6 days then the itinerary may not be all consecutive days
The Post Heart Attack Stem Cell Treatment at Dream Body Clinic
At Dream Body Clinic, we understand how devastating a heart attack (myocardial infarction) can be to your quality of life. That’s why we’ve developed an effective treatment option utilizing advanced stem cell therapy to help improve your heart function and overall quality of life.
Our Post Heart Attack Stem Cell Treatment is a cutting-edge regenerative medicine therapy designed to promote natural healing and regeneration in the heart. This treatment involves the use of mesenchymal stem cells, which have been shown to improve heart function by reducing inflammation, promoting tissue repair, and modulating the immune response.
Our team of expert medical professionals has extensive experience in administering this stem cell therapy. We use Wharton Jelly (umbilical cord tissue) and placenta to derive our pure, isolated MSCs. Then we cultivate them to get the hundreds of millions necessary for this advanced treatment. The MSCs are then safely infused into your body to facilitate natural healing and regeneration.
Our Post Heart Attack Stem Cell Treatment offers several benefits, including:
- Improved heart function and reduced symptoms of Congestive Heart Failure (CHF)
- Reduced inflammation and improved circulation in the heart
- Regeneration of damaged heart tissue
- Minimal recovery time and no hospital stay
- Safe and effective treatment with few side effects
If you’re seeking an innovative, non-invasive treatment for your heart regeneration, our Post Heart Attack Stem Cell Treatment is an excellent option. At Dream Body Clinic, we’re dedicated to providing personalized and effective regenerative medicine therapies that help you achieve optimal health and wellness. Contact us today to learn more about this life-changing treatment option.
Call (888) 704-3977 For a Free Consultation
You can also email us at info@dreambodyclinic.net
How do Mesenchymal stem cells work for Post Heart Attack Recovery?
Mesenchymal stem cells (MSCs) have been shown to have beneficial effects in the treatment of Post Heart Attack through multiple mechanisms:
Anti-inflammatory effects: MSCs have immunomodulatory properties and can reduce inflammation in the heart, which is a key contributor to Congestive Heart Failure (CHF). They can also reduce oxidative stress and prevent cell death.
Promotion of tissue repair: MSCs can guide various types of cardiovascular cells to promote angiogenesis and guide the formation of new blood vessels.
Improvement of cardiac function: MSCs can increase cardiac output and improve left ventricular function in patients with CHF.
Reduction of fibrosis: MSCs can reduce fibrosis or scarring in the heart, which is a common consequence of CHF.
Overall, MSCs have the potential to address multiple aspects of Post Heart Attack recovery and are probably the best treatment option available.
How do Mesenchymal Stem Cells Reduce Heart Inflammation for Post Heart Attack Recovery?
Mesenchymal stem cells (MSCs) have been shown to reduce inflammation in the heart through several mechanisms:
Secretion of anti-inflammatory molecules: MSCs can secrete various anti-inflammatory molecules, such as interleukin-10 (IL-10), transforming growth factor-beta (TGF-β), and prostaglandin E2 (PGE2). These molecules inhibit the activity of immune cells and reduce inflammation.
Suppression of immune cell activity: MSCs can inhibit the activity of immune cells, such as T cells and B cells, that contribute to inflammation in the heart.
Modulation of macrophage polarization: MSCs can regulate macrophage polarization, which is important for inflammatory responses. They can induce macrophages to adopt a pro-resolving (anti-inflammatory) phenotype, which further reduces inflammation.
Reduce oxidative stress: MSCs can also reduce oxidative stress, which is a key contributor to inflammation in the heart. They can scavenge free radicals and promote antioxidant defense mechanisms, reducing the inflammatory response.
Overall, MSCs have demonstrated their ability to reduce inflammation in the heart through complex mechanisms that target various aspects of the inflammatory response. The most amazing thing is that the stem cells know where to send exosomes with the needed cytokines, chemokines and trophic factors needed to guide the healing. Without this precision delivery service the exosomes would just be free floating and have little therapeutic effect. MSCs are like your bodies own emergency medical team that responds appropriately to the environment and sends out the correct signals to guide healing.
How does interleukin-10 reduce heart inflammation?
Mesenchymal Stem Cells will seek out inflammation of the heart and then release exosomes that carry Interleukin-10 to the damaged area. Interleukin-10 (IL-10) is an anti-inflammatory cytokine that plays a crucial role in reducing heart inflammation. IL-10 is secreted by various immune cells, including T cells, B cells, and macrophages.
IL-10 works by suppressing the activity of pro-inflammatory immune cells and promoting the activities of anti-inflammatory cells. It can inhibit the production of pro-inflammatory cytokines, such as interleukin-1 beta (IL-1β), tumor necrosis factor-alpha (TNF-α), and interferon-gamma (IFN-γ).
In the context of Post Heart Attack Recovery, IL-10 can reduce inflammation of the heart by:
Suppressing the activity of immune cells: IL-10 can inhibit the activity of pro-inflammatory immune cells, such as macrophages and T cells, that promote inflammation in the heart.
Downregulating Toll-like receptor (TLR) signaling: IL-10 can inhibit TLR signaling, which is important for the activation of immune cells that trigger inflammation.
Inducing anti-inflammatory immune cells: IL-10 can promote the activity of anti-inflammatory immune cells, such as regulatory T cells (Tregs), that can suppress inflammation.
Reducing oxidative stress: IL-10 can also reduce oxidative stress, which can contribute to inflammation in the heart. It can promote antioxidant defense mechanisms and scavenge free radicals.
Overall, IL-10’s anti-inflammatory effects make it an amazing therapeutic target for CHF and other cardiovascular diseases.
How does transforming growth factor-beta reduce heart inflammation?
Mesenchymal Stem Cells will seek out inflammation of the heart and then release exosomes that carry Transforming growth factor-beta (TGF-β) to the damaged area. Transforming growth factor-beta (TGF-β) is a cytokine that plays a crucial role in reducing heart inflammation. In the context of Post Heart Attack Recovery, TGF-β reduces inflammation of the heart by:
Inhibiting pro-inflammatory cytokine production: TGF-β can inhibit the production of pro-inflammatory cytokines, such as interleukin-1 beta (IL-1β), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α), that contribute to heart inflammation.
Promoting anti-inflammatory cytokine production: In addition to inhibiting pro-inflammatory cytokines, TGF-β can also promote the production of anti-inflammatory cytokines, such as interleukin-10 (IL-10), that can help to reduce inflammation in the heart.
Inducing immune tolerance: TGF-β can induce immune tolerance, which can help to prevent the immune system from overreacting and causing damage to the heart. This is achieved through the suppression of effector immune cell function and promotion of regulatory T cell (Treg) function.
Modulating extracellular matrix (ECM) deposition: TGF-β plays a role in the deposition of the ECM, which provides structural support to the heart. Inflammation in the heart can lead to excessive ECM deposition and fibrosis, which can impair heart function. TGF-β can modulate this process, helping to prevent excessive ECM deposition and fibrosis.
Overall, TGF-β plays a significant role in regulating inflammation in the heart and can have beneficial effects in reducing heart inflammation post heart attack.
How does prostaglandin E2 reduce heart inflammation?
Mesenchymal Stem Cells will seek out inflammation of the heart and then release exosomes that carry Prostaglandin E2 (PGE2) to the damaged area. Prostaglandin E2 (PGE2) is an important lipid mediator that plays a key role in reducing inflammation in the heart. In the context of Post Heart Attack Recovery, PGE2 can reduce inflammation of the heart by:
Suppressing pro-inflammatory cytokines: PGE2 can inhibit the production of pro-inflammatory cytokines, such as interleukin-1 beta (IL-1β) and tumor necrosis factor-alpha (TNF-α), that contribute to inflammation in the heart.
Promoting anti-inflammatory cytokines: PGE2 can stimulate the production of anti-inflammatory cytokines, such as interleukin-10 (IL-10), which can help to reduce inflammation.
Modulating immune cell activity: PGE2 can modulate the activity of immune cells, including macrophages, dendritic cells, and T cells, to reduce inflammation. PGE2 can promote the activity of anti-inflammatory immune cells while inhibiting pro-inflammatory immune cells.
Reducing oxidative stress: PGE2 can also reduce oxidative stress in the heart, which can contribute to inflammation. It can promote antioxidant defense mechanisms and scavenge free radicals.
Overall, PGE2’s anti-inflammatory effects make it an effective therapeutic target for CHF and other cardiovascular diseases. In fact, some studies have shown that treatment with PGE2 can improve heart function and reduce inflammation post heart attack.
How do mesenchymal stem cells guide the regeneration of damaged heart tissue in Post Heart Attack Recovery?
Mesenchymal stem cells (MSCs) can guide the regeneration of damaged heart tissue post heart attack. It takes a combination of several mechanisms to regenerate damaged heart tissue. The following are the mechanisms used to do it:
Paracrine signaling: MSCs can secrete various factors that promote tissue repair, such as growth factors, cytokines, and extracellular vesicles. These factors can stimulate the growth and differentiation of resident stem cells and progenitor cells, leading to the regeneration of damaged heart tissue.
Promotion of angiogenesis: MSCs can also promote angiogenesis or the formation of new blood vessels in damaged heart tissue. This is important for bringing oxygen and nutrients to the site of injury and supporting tissue repair.
Modulation of the immune response: MSCs can modulate the immune response to the damage, reducing inflammation and promoting a pro-regenerative environment.
Regeneration of Contractile Cells: MSCs have the potential to guide various types of cardiovascular cells, including cardiomyocytes which are contractile cells that compose the heart muscle. Some studies thought that MSCs could differentiate into cardiomyocytes and regenerate the damaged heart tissue because the regeneration was incredible. It was later established in further studies that they simply guide the cardiomyocytes in combination with the other mechanisms listed here to regenerate the damaged heart.
ECM remodeling: MSCs can also contribute to the remodeling of the extracellular matrix (ECM) in damaged heart tissue, which is important for creating an environment that supports tissue repair.
Overall, the ability of MSCs to guide tissue repair in the heart is the most effective therapeutic strategy for CHF and other cardiovascular diseases.
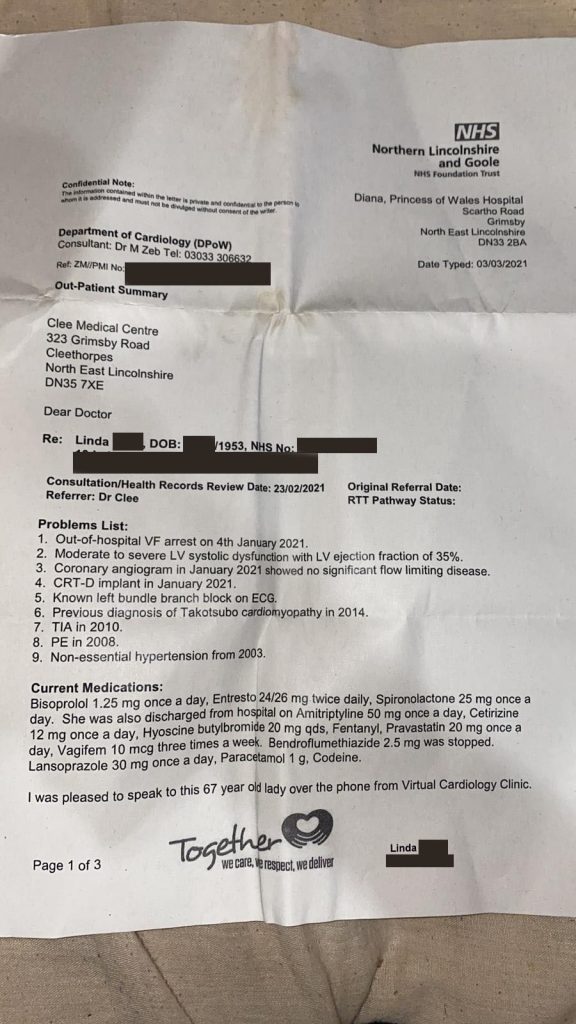
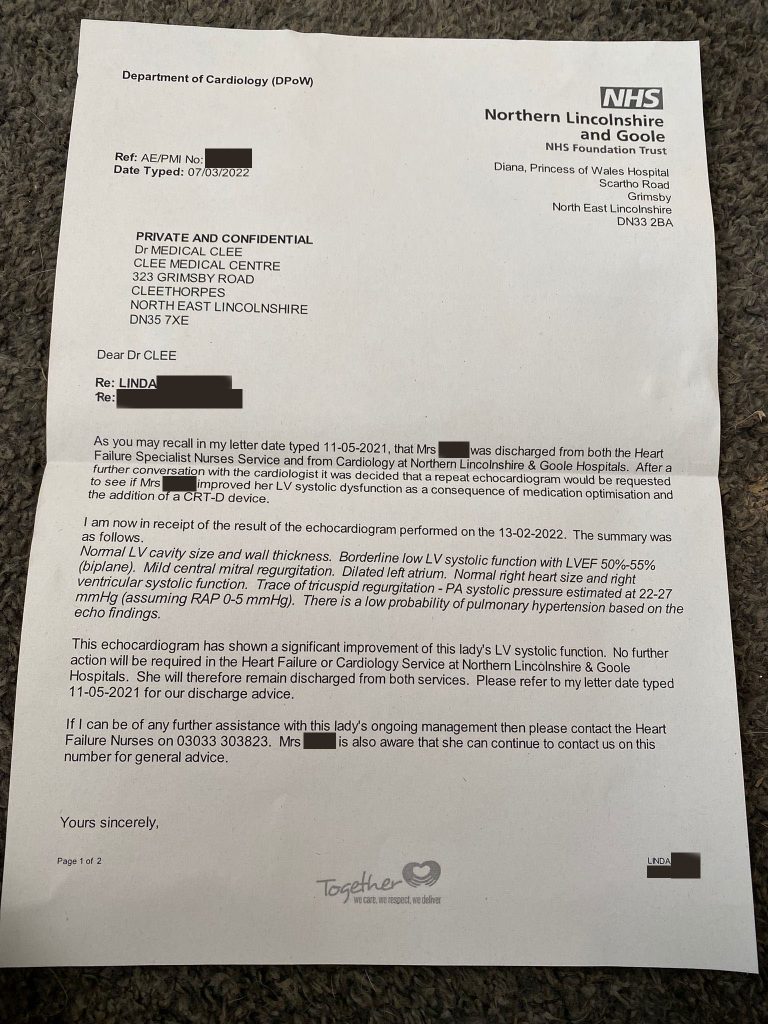
Patient Ejection Fraction goes from 35% to 55% at 3 months post Stem Cell Therapy at Dream Body Clinic
Mesenchymal Stem Cells Heart Disease Studies
- Mesenchymal Stem Cells in Cardiovascular Regeneration
- Mesenchymal Stem Cell Therapy for Cardiac Inflammation
- Multimodality Noninvasive Imaging Demonstrates In Vivo Cardiac Regeneration After MSC Therapy
- Human Umbilical Cord Mesenchymal Stem Cells: A New Era for Stem Cell Therapy
- mesenchymal stem cell-released paracrine factor mediating myocardial survival and repair
- Exosome secreted by MSC reduces myocardial ischemia/reperfusion injury
- Use of Mesenchymal Stem Cells for Therapy of Cardiac Disease
- Therapeutic Application of Mesenchymal Stem Cells Derived Extracellular Vesicles for Immunomodulation
- Double blind, placebo controlled study of MSCs application post Heart Attack
- Safety and Efficacy of the Intravenous Infusion of Umbilical Cord Mesenchymal Stem Cells in Patients With Heart Failure: A Phase 1/2 Randomized Controlled Trial
- Mesenchymal stem cell therapy for heart failure: a meta-analysis
- Safety and Efficacy of Adult Stem Cell Therapy for Acute Myocardial Infarction and Ischemic Heart Failure
- Mesenchymal Stem Cells in Fibrotic Disease
- Immunomodulatory effects of human umbilical cord Whartons jelly-derived mesenchymal stem cells on differentiation maturation and endocytosis of monocyte-derived dendritic cells
- The immunosuppressive potential of mesenchymal stem cells
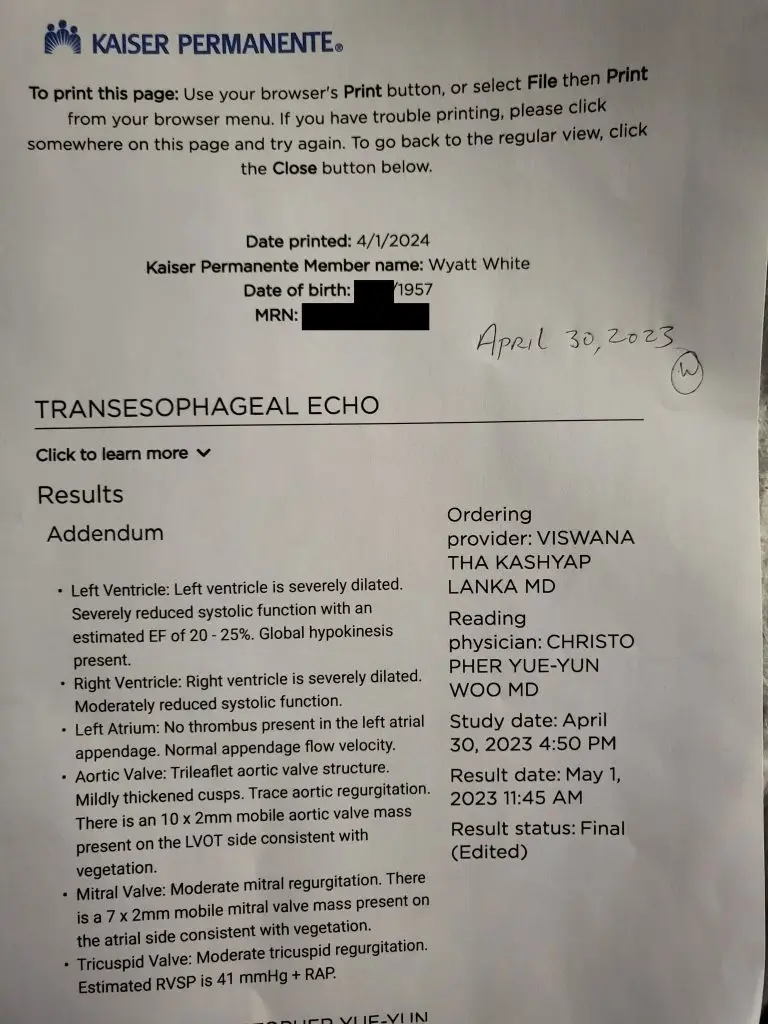
Patient Ejection Fraction goes from 25% to 60% at 1 Year
post Stem Cell Therapy at Dream Body Clinic
Side Effects or Risks
The only side effects that have been documented are the following:
- 1 in 100 people will experience a slight fever and/or headache for a few hours after treatment or the next day. We have found that 500mg of Tylenol easily resolves this issue.
- Any treatment involving an injection such as an IV runs a risk of infection. We have never had a patient experience an infection due to our sterility protocols,.
- We do not treat patients that have had cancer within the past 5 years. There is still no conclusive evidence linking stem cells to make cancer worse, but we prefer to stay on the side of safety until more information is available.
- The heart tends to have more fluid around it for patients with congestive heart failure so we must be sure that the patient is fit for treatment. A patient could experience increased blood pressure from treatment so we take care to run EKG, echocardiogram and chest x-rays before treatment then have that reviewed by our cardiologist and internist.
- We do not recommend traveling to Dream Body Clinic via airplane if your ejection fraction is below 30% because the increased elevation while flying can cause heart issue and blood pressure issues.
- As with any medical treatment there is no guarantee of results, but our outcomes have been great for the vast majority of patients.
- In all patients who receive an intravenous treatment of any sort, there is a risk of releasing a thrombus or plaque from the veins, even more so if the patient has mainly high cholesterol levels. If a thrombosis or phlebitis were to occur, it would occur immediately. This has not been an issue with our patients, but any sort of IV has this risk. This is why we do bloodwork for all patients to make sure that treatment is as safe as possible for them.
Our lab has over 8 years of experience cultivating mesenchymal stem cells with perfect safety and efficacy. See Stem Cell Certification by Clicking Here
How long do the Post Heart Attack Stem Cell Treatment Results Last?
The results from the Post Heart Attack stem cell treatment can last for years or even indefinitely. This is because the stem cells are creating real cellular regeneration. Any improvement to your heart tissue will last because it is new heart tissue. The stem cells will also reprogram your immune system to work the way it was designed to work. Once the immune cells are reprogrammed and any damage is repaired at the heart then things will work the way they should. This will last because it is real regeneration and not just a pill to cover up symptoms.
The mesenchymal stem cells that are administered via IV will stay in the system for 8 months to a year. During that time they will interact with immune cells and seek out inflammation where they will guide cellular regeneration. After 8 to 12 months any MSCs that are free bound in your system will differentiate into an osteoblast (bone cell), adipocyte (fat cell) or chondrocyte (cartilage cell). They will then contain the donors HLA markers and your immune system will destroy and remove them. This is an easy process for your immune system and there is no negative reaction in your body from it. Some of the MSCs that were free bound from the IV will find capillaries to call home. They will attach and be considered a pericyte. When they do this they can live in your system indefinitely in a beneficial way to your system.
The Post Heart Attack Stem Cell Treatment is allowing your body to heal like it did when you were a little kid.
How to get the Post Heart Attack Stem Cell Treatment
In conclusion, the Post Heart Attack stem cell treatment could be a promising solution for individuals who are facing this condition. The Dream Body Clinic provides personalized treatment plans using stem cells to repair and regenerate damaged tissues of the heart, which may lead to improved increased ejection fraction and overall heart function. While this treatment is not yet widely available, ongoing research suggests that it could be a viable alternative to traditional Post Heart Attack management methods. If you are interested in learning more about this treatment, we recommend calling us for a free consultation at (888) 704-3977. If you are ready to get the Post Heart Attack Stem Cell Treatment then click the image below for details on how to book.