The following information was written by Dr. Liji Thomas, MD about, Could Mesenchymal Stem Cells improve the outcomes of ARDS in Severe COVID-19 Cases?
The 2019 coronavirus disease (COVID-19) pandemic has been associated with hundreds of millions of hospitalizations and more than 3.2 million deaths since it first emerged in late 2019. While severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) primarily causes asymptomatic or mild disease, in approximately 15% of cases, patients become moderately or severely ill.
A recent study, published in Stem Cells Translational Medicine, explores the safety and efficacy of stem cells, which have been touted as the panacea for a wide range of diseases, ranging from chronic degenerative diseases to cancer.
The severity of COVID-19 in some patients appears to be due to a hyperinflammatory state resulting from a deregulated immune response. This is characterized by a storm of cytokines and immunologically mediated clots. A distressing and often fatal complication of critical COVID-19 is acute respiratory distress syndrome (ARDS), often associated with multiorgan dysfunction.
Therapies are now needed to reduce the severity of inflammation, which can shorten the vicious cycle that shortens the survival of these patients. Corticosteroids have been shown to have significant use under specific conditions.
It is argued that the use of stem cells in this scenario is of potential benefit in modulating immune responses in patients with severe COVID-19. Researchers in this study obtained umbilical cord mesenchymal stem cells (UC-MSC), which can proliferate rapidly for clinical use and have been reported to be safe in other conditions.
These stem cells are not subject to ordinary host-graft incompatibility conditions and have been used in various autoimmune and inflammatory diseases. Approval has been granted by the U.S. Food and Drug Administration. For the use of UC-MSC for type 1 diabetes and Alzheimer’s disease.
Objectives and findings of the study
Some studies have shown good results in patients with COVID-19 pneumonia who were treated with MSC who do not express the angiotensin-converting enzyme 2 (ACE2) from the host cell molecule that serves as the virus receptor. This stimulated current research on the safety and efficacy of UC-MSC as a therapy for ARDS in patients with COVID-19.
Conducted as a blinded randomised controlled trial, it was designed as a phase 1/2a trial in 24 patients. First, it was observed that the use of these stem cells was safe. While more than 90% of patients in the treatment group survived 28 days from the last dose, only 42% in the control group did.
Possible explanations
The key effects of stem cell treatment are to reduce the levels of inflammatory mediators such as interferon (IFN)-γ, interleukin (IL)-6, and tumor necrotic factor (TNF)-α, which play a central role in the COVID-19 cytokine storm. Simultaneously, they reduce levels of granulocyte-monocyte colony-stimulating factor (GM-CSF), the main activator of the process by which monocytes are activated to become proinflammatory M1 macrophages. By doing so, they can shift the balance towards M2 macrophages that are activated by another route.
Levels of PDGF-BB (a type of platelet-derived growth factor with two B subunits), which powerfully stimulates cells of mesenchymal origin, were also reduced. This mediator improves the activation of mesenchymal cells, stimulates the proliferation and migration of smooth muscle cells of the airways, increases the production of cytokines in pulmonary fibroblasts and activates pain-sensitive neurons.
Therefore, a reduction in PDGF-BB levels could mean that MSC therapy accelerates the tissue repair process, thus accelerating recovery in the lungs, reducing the need for increased PDGF-BB secretion.
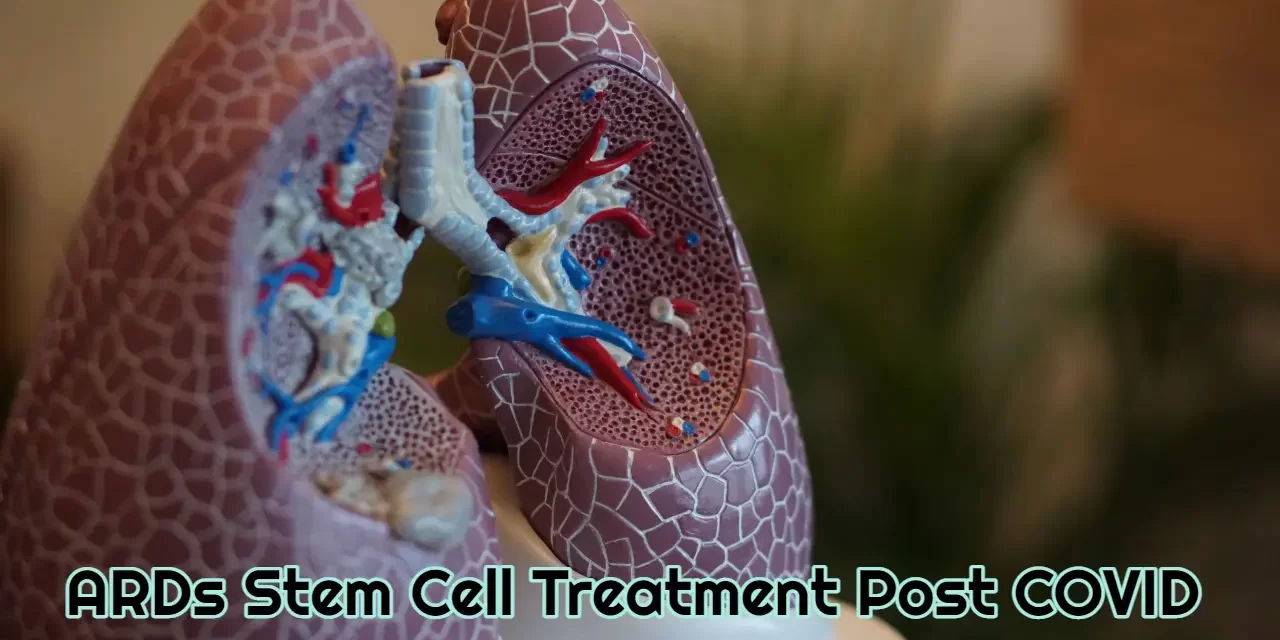
Acute Respiratory Distress Syndrome ARDS Stem Cell Treatment
Acute Respiratory Distress Syndrome ARDS Stem Cell Treatment is a stem cell therapy done with an 200 million stem cell IV followed by 4 sessions of 25 million nebulized stem cells. ARDS is one of those diseases that doctors currently can only manage the symptoms after lung failure. Mesenchymal Stem Cells flip this paradigm as they have now been found to treat ARDS with great success. When Mesenchymal Stem Cells (MSCs) are administered via IV they go directly to the lungs first. This is called the first pass and a great thing for ARDS as the majority of the stem cells (approximately 80%) never get past the lungs and heart. The stem cells are attracted to inflammation and the lungs are full of it. They get to work by guiding the removal of fibrosis (scarring) and then guiding the cellular repair. ARDS typically leaves patients with severely damaged lungs and no way to repair and regenerate. The MSCs are able to help you get your breath back.
To get started please fill out our intake form and then we will call for a free consultation – INTAKE FORM
Intranasal Stem Cell Application Study
https://www.sciencedirect.com/science/article/pii/S0014488614001964
Intranasally administered mesenchymal stem cells promote a regenerative niche for repair of lung damage. This study shows that intranasal stem cell application helps heal the lungs and brain. We prefer to use a nebulized approach for intranasal application as more stem cells are able to get to the mucus membrane and pass to the blood stream to go straight to the brain.
TREATMENT PROTOCOL
- Blood Panel to give you a baseline to compare and measure effects
- 200 million mesenchymal stem cells administered at 100 million per day over the course of 2 days
- 25 million mesenchymal stem cells administered via nebulization twice a day for 2 days for a total of 100 million
- Lyophilized placenta injection
The first day you arrive is to settle in and rest. You fast that night and next morning until we do a blood panel around 8 or 9am. We also need to know what medications you are on as some medications need to be stopped for a few days leading up to this treatment. For the stem cells we need you to stop taking any Nonsteroidal anti-inflammatory drugs (NSAIDs) a week before getting stem cell treatment. You can use them afterwards. The most prominent NSAIDs are aspirin, ibuprofen and naproxen Here is a breakdown of what NSAID’s – https://en.wikipedia.org/wiki/Nonsteroidal_anti-inflammatory_drug. We need at least 3 day notice to have treatment ready for you as the cells are only viable for 4 days from when we receive them.
Side Effects or Risks
The only side effects that have been documented are the following:
- 1 in 100 people will experience a slight fever and/or headache for a few hours after treatment or the next day.
Our lab has over 8 years specializing in Mesenchymal Stem Cell research. Our lab has done a maximum of 1 billion stem cells via IV with no negative side effects. See Stem Cell Certification by Clicking Here.
As with any medical treatment, there is no guarantee of success.
Studies into MSCs for ARDS
- Mitochondrial Transfer via Tunneling Nanotubes is an Important Mechanism by which Mesenchymal Stem Cells Enhance Macrophage Phagocytosis in the in vitro and in vivo Models of ARDS
- Treatment with allogeneic mesenchymal stromal cells for moderate to severe acute respiratory distress syndrome (START study): a randomised phase 2a safety trial
- Cell therapy in acute respiratory distress syndrome
- Mesenchymal stem (stromal)cells for treatment of ARDS: a phase 1 clinical trial
- Nebulized Stem Cells – Airway delivery of conditioned media from mesenchymal stem cells (MSC-CM) for COPD
- Therapeutic potential of products derived from mesenchymal stem/stromal cells in pulmonary disease
- Therapeutic potential of airway remodeling with MSCs
Why do we need Mesenchymal Stem Cells?
We need more stem cells as we age, but our body is using them up. When we are infants, we have the most stem cells that we will ever have and then by the time we grow up to bone maturity, we only have 10% of these cells left. Only 10% and that is all we have left to work with for the rest of our lives. Cells die off as we age and that percentage goes down even further every year.
So How do Mesenchymal Stem Cells Work?
Mesenchymal Stem cell therapies work by stimulating the body to regenerate itself. Their magic is not in their ability to become or replace different tissues or cells, but in their production of trophic factors, bioactive molecules produced in response to the environment in which the cells are in. These secreted chemicals aid in repairing tissue and the recruitment of new blood vessels to support nutrient flow to the area and decrease inflammation. By repairing tissue, recruiting new blood vessels and increased nutrient flow your body will start to behave the way it is meant to operate. So it is not the cells themselves that work the magic. It is what the cells secrete that has such medicinal potential.
Only available at our Puerto Vallarta Stem Cells clinic. Puerto Vallarta stem cell treatment.
More info on the Mesenchymal Stem Cell Secretions
Mesenchymal Stem cells (MSCs) secrete a wide range of cellular products, molecules, exosomes (part of the genome thats inside RNA. Progams protein coding) and microvesicles ( Microvesicles play a role in intercellular communication and can transport mRNA, miRNA, and proteins between cells.) That act in different ways to stimulate the body’s healing process.
Growth Factors Aid in Healing
Growth factors (A growth factor is a naturally occurring substance capable of stimulating cellular growth, proliferation, healing, and cellular differentiation. Usually it is a protein or a steroid hormone. Growth factors are important for regulating a variety of cellular processes. Cytokines (Cytokines are a broad and loose category of small proteins that are important in cell signaling. Their release has an effect on the behavior of cells around them. It can be said that cytokines are involved in autocrine signaling, paracrine signalingand endocrine signaling as immunomodulating agents.) , hormones, and cellular mitochondria and RNA are among the secreted bioactive molecules and cellular material that characterize the wide range of activities carried out by mesenchymal stem cells. When considering that the main function of stem cells lies in their secretome. This is the bioactive molecules they secrete. This means they don’t have the ability to differentiate into new tissue, but intead allow your own body to heal itself properly. Isolating these trophic factors separate from the cells offers an intriguing mode of treatment.
Puerto Vallarta stem cell treatment for Acute Respiratory Disease Treatment
Do the Mesenchymal Stem Cell Treatment Results Last?
The results from 200 million stem cell IV + 4 nebulized sessions are lasting because your body is able to heal itself like when you were younger. That healing does not go away fast, just think of how many years it took to get you where you are. By getting this treatment once or twice a year, your body will be able to regenerate more and more. The 300 million cells will stay in your system until they mature after a year. Many will find capillaries to call home and those can stay with you indefinitely. So any extra capillary space available is filled with the stem cells and they stay with you. The rest of the stem cells circulate in your blood stream looking for areas of inflammation and cells to help. Mesenchymal stem cells are the only cells that have been found able to donate mitochondria to weak or injured cells, thus making them whole again. The stem cells that don’t find a home in your capillaries stay for up to 8 months at which time they mature and your body flushes them out.
Call us at (833) 445-9089 for a Free Consultation about the ARDs Stem Cell Treatment Now!